Our laboratory studies many different forms of neonatal brain injury, focusing on pathophysiology, biomarkers, prediction modeling and neuroprotection strategies.
Advances in neuroprotection
Long term neurodevelopmental outcome is the primary concern cited by parents of infants admitted to the NICU. All neonates in the NICU are at increased risk for a number of different forms of brain injury. Through single center and collaborative efforts, we are dedicated to discovering new methods for protecting the vulnerable neonatal brain and proving efficacy through high quality clinical trials.
Applications of MR imaging in the newborn
Advanced imaging using MRI can provide unique and powerful insights into structural brain injury and can aid in predicting long term neurodevelopmental outcome. However, the interpretation of the MRI is not straightforward. Using quantitative MRI techniques in conjunction with machine learning technology, we aim to improve the quality and accessibility of predictive modeling.
Anemia of prematurity
Anemia of prematurity is a ubiquitous problem in the NICU, nearly every preterm infant born before 28 weeks gestation will receive at least one transfusion during the course of their hospitalization. Nevertheless, thresholds for transfusion and transfusion related practices (such as withholding feed) remain controversial. Using longitudinal physiologic studies with NIRS and other vital sign data, we hope to develop patient specific transfusion thresholds and a better understanding of the body’s response both to anemia and the transfusion.
Blood pressure and transitional hemodynamics
The days following birth are a challenging period for premature neonates. This transitional period may be marked by respiratory failure and hypoxia, poor cardiac function and hypotension and significant apnea. Current clinical practice uses outdated definitions for hypotension and largely subjective and ephemeral assessments of physiology. Computational analysis of vital signs can reveal quantitative physio markers which not only predict future adverse clinical events but also provide markers of response to treatment.
Cerebellar hemorrhage
Cerebellar hemorrhage (CH) is one of the three forms of brain injury faced by premature infants. Difficult to diagnose without specialized imaging, CH has the potential to have a major impact on neurodevelopmental impair. Historically, CH is far less studied that the two more common forms of preterm brain injury (intraventricular hemorrhage and white matter injury) — a gap we aim to close.
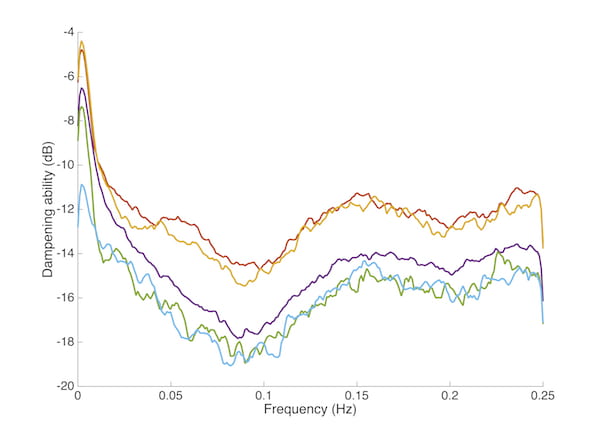
Cerebral autoregulation
The human brain contains a complex regulatory system which is intended to provide a smooth, consistent blood flow supply, regardless of the physical position of the body or other physiologic disruptions. Autoregulatory function can be disrupted by brain injury and may not be fully mature in the case of premature infants. In a series of studies, we have focused on defining and quantifying cerebral autoregulation in neonates. Our long term plan is to identify strategies for manipulation of autoregulatory function to provide targeted therapeutics and reduce brain injury risk.
Disparities in neonatal care
It is well known that African American women are more likely to have premature infants than women of other ethnicities. There is significant concern that many of the monitoring and treatment paradigms used in the NICU may contain hidden biases and provide suboptimal care for non-Caucasian infants. We explore how these disparities might exist in all aspects of neonatal care and strive to eliminate these issues.
Ductus arteriosus physiology
A patent ductus arteriosus is a common and confounding problem in many premature infants. There is broad diversity in opinion about the correct course of management and implications for long term outcomes. We hope to answer many of these questions and aid in the understanding of less invasive treatment options.
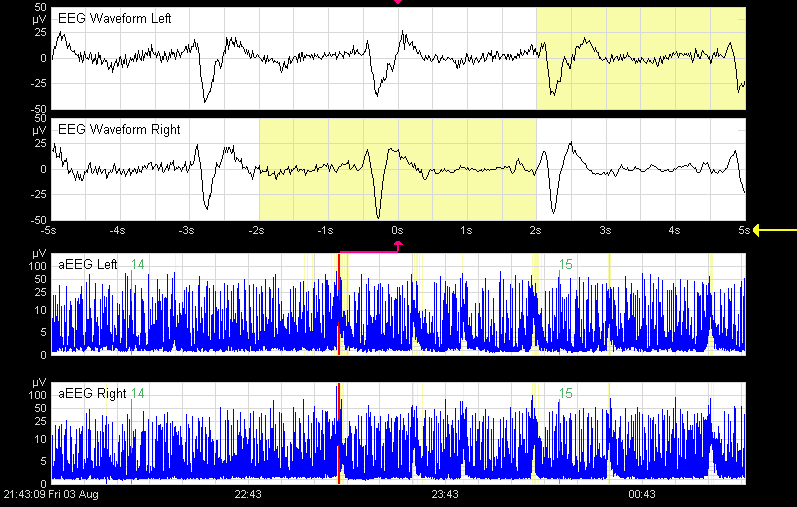
EEG analysis and seizures
EEG is an important technology for understanding brain function and detecting seizures. Our lab is focused on improving quantitative reproducible measures of EEG to detect seizure and predict injury. We have published an open-source toolbox of EEG analysis algorithms and continue to push for the development of accessible monitoring technologies to reduce disparities in neonatal neurocritical care.
Hypoxic-ischemic encephalopathy
Hypoxic-ischemic encephalopathy (HIE) is the most common form of brain injury affecting term born neonates and results from a temporary reduction in cerebral blood flow during the perinatal period.
Our research investigates HIE from a number of different angles including a new approach to brain MRI scoring, validated against long-term follow-up data, investigation into dysfunction of the cerebrovascular autoregulatory system in HIE and new extensions of the neuroprotective treatment, therapeutic hypothermia in new patient populations than previously studied.
We are also a recruiting center for the multicenter trial of EPO for neuroprotection in HIE and form the neuroimaging core (with Bob Mckinstry, MD, PhD) for the study that will include 500 infants.
Intraventricular hemorrhage

Intraventricular hemorrhage (IVH) is the most common form of brain injury in infants born before 28 weeks of gestation.
Our lab is currently investigating how disturbances in perfusion alter the risk for IVH. In particular, this work focuses on models of cerebrovascular autoregulation using simultaneous collection of physiology data in conjunction with near-infrared spectroscopy measurements of cerebral perfusion.
Recently we published a novel measurement of autoregulation which demonstrates that autoregulation improves with maturation and infants with IVH have impaired autoregulation.
NAS/NOWS
Neonatal abstinence syndrome (NAS) sometimes called neonatal opioid withdrawal syndrome (NOWS) has increased exponentially in the last decade and is a leading reason for admission to the NICU. Through a combination of clinical studies, physiologic studies and clinical trials, we hope to improve the consistency of evaluation, optimize treatment and reduce barriers to care.
Neonatal-perinatal medicine
In addition to neurology focused studies, we are dedicated to improving all neonatal care. In a mix of QI initiatives and clinical research, we strive to be understand how infants get sick, what interventions provide optimal improvement and the best strategies for encouraging adoption of new methods of care.
Neonatal sepsis
Early and late onset sepsis are significant sources of neonatal morbidity and mortality. Although the blood culture is the gold standard for detection of sepsis and identification of organisms, early warning systems which can identify sepsis with a high degree of specificity 12 or more hours earlier allow the potential for intervention and a consequential reduction in morbidity and mortality. Through single center and collaborative projects, we are developing physiomarkers for sepsis using computational methods to provide effective early warning systems.
Retinopathy of prematurity
Retinopathy of prematurity (ROP) is a common form of visual impairment in premature neonates. Although the development of ROP has been linked to oxygen exposure, previous trials have failed to demonstrate a consistent, reproducible measure for assessing risk.
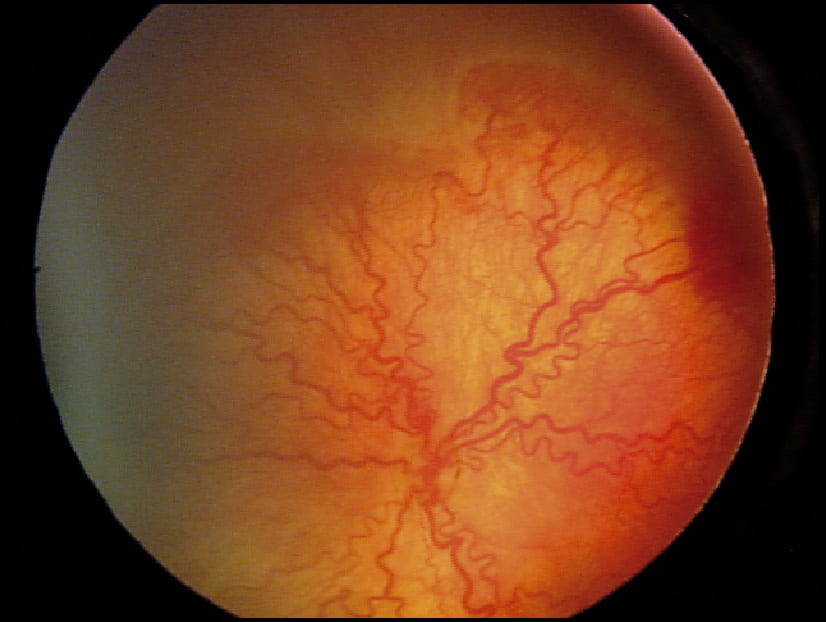
Recent work done by our lab developed a new, multimodality approach for measuring oxygenation which has shown promised in reliably predicting the risk of ROP, as compared to existing technology.
White matter injury
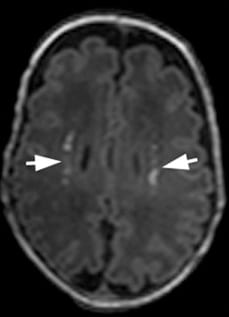
White matter injury — periventricular leukomalacia — is another common form of brain injury in premature neonates born before 28 weeks of gestation and is linked to the subsequent development of cerebral palsy.
Our lab has developed new approaches to the quantification of white matter injury on MRI, prediction of white matter injury using EEG and longitudinal evaluation of cerebral blood flow disturbances and the development of white matter injury.
Recent work by our lab has demonstrated that a simple, limited channel bedside EEG is capable of predicting white matter injury on MRI.